Recent budget plans from House Republicans have sparked heated debate on the future of healthcare. Let’s look at these substantial changes and their far-reaching implications for American families.
Major changes in the Healthcare Budget
America’s healthcare spending is about to undergo a seismic upheaval. House Republicans have suggested eliminating $1.5 trillion from the federal budget. Healthcare systems, particularly Medicare and Medicaid, are set to lose significant money.
The new budget framework suggests deep cuts to established healthcare systems. While advocates argue that these measures will cut government spending, detractors point to potential gaps in care. Health policy specialists warn about the long-term consequences for public health.
These cuts could change the way states administer their healthcare programs. Some projections predict that Medicaid might face cuts of up to $880 billion. This statistic has provoked fierce debate in Congress and beyond.
Impact on Everyday Americans
The proposed changes could affect millions of Americans. Working families depending on Medicaid might face reduced coverage options. Senior citizens relying on Medicare could see changes in their benefits and coverage terms.
Some significant effects might include:
– Reduced funding for essential health services
– Extended wait times for medical procedures
– Increased out-of-pocket costs for prescriptions
– Limited coverage for specialized treatments
– Higher insurance premiums for many families
– Fewer preventive care options
Healthcare providers across the nation express serious concerns. Many hospitals worry about maintaining quality care with reduced funding. Rural healthcare facilities might face particular challenges in serving their communities.
Changes to Social Programs and Healthcare Access
Healthcare providers across the country voice major worries. Many hospitals are concerned about maintaining quality care despite lower financing. Rural healthcare facilities may confront unique problems while serving their communities.
State governments face tough choices ahead. They might need to:
– Increase state taxes to maintain services
– Reduce coverage for optional Medicaid services
– Limit enrollment in health programs
– Cut payments to healthcare providers
– Find new ways to fund emergency services
How Communities Are Preparing
Local organizations and communities are developing strategies to cope. Many families have started planning for potential changes. Community health networks are expanding their support systems.
Practical steps people are taking include:
– Researching alternative insurance options
– Creating emergency medical savings funds
– Connecting with local health resources
– Scheduling important procedures before changes take effect
– Learning about preventive health measures
– Building support networks for medical emergencies
Working with Healthcare Providers in a Changing Landscape
Medical professionals are adapting their practices. Many doctors’ offices are:
– Developing sliding scale payment options
– Creating new efficiency measures
– Expanding telehealth services
– Forming partnerships with community organizations
– Implementing cost-saving technologies
Community health centers are preparing for increased demand. These facilities often provide crucial services to underserved populations. Their role might grow more important as traditional healthcare becomes more expensive.
Financial Planning and Healthcare
Americans are learning to think differently about health costs. Financial advisors suggest several strategies:
– Building larger emergency funds
– Understanding insurance alternatives
– Exploring health sharing ministries
– Investigating prescription assistance programs
– Planning for long-term care needs
Looking Ahead: Policy and Practice
The healthcare landscape continues to evolve. Lawmakers debate various approaches to budget management. Healthcare organizations prepare for multiple scenarios.
Key areas of focus include:
– Protecting essential medical services
– Maintaining access to preventive care
– Supporting vulnerable populations
– Balancing cost control with quality care
– Developing sustainable funding models
Impact on Different Demographics
Various groups face unique challenges:
Seniors:
– Possible changes to Medicare coverage
– New costs for prescription drugs
– Different options for supplemental insurance
Working Families:
– Changed eligibility for assistance programs
– New insurance marketplace dynamics
– Different employer healthcare options
Low-Income Individuals:
– Altered Medicaid accessibility
– Changed qualification requirements
– New barriers to care
State-by-State Variations
Healthcare changes won’t affect all states equally. Some states plan to create safety nets. Others might struggle to maintain current service levels.
Key differences include:
- States with expanded Medicaid face bigger adjustments
- Rural states might see more hospital funding challenges
- Some states prepare special healthcare funds
- Coastal states explore multi-state healthcare partnerships
- Different approaches to preventive care programs
Healthcare Industry Response
Medical providers are developing new service models. These changes aim to keep care accessible despite budget cuts.
Industry adaptations include:
- Group medical practices joining forces
- Hospitals creating mobile health units
- New payment models for routine care
- Expanded use of nurse practitioners
- Innovation in remote health monitoring

Mental Health Services Impact
Mental health coverage faces unique challenges. Budget cuts might affect these essential services differently than physical health care.
Key concerns include:
- Changes to counseling coverage
- Medication assistance programs
- Support group funding
- Crisis intervention services
- Prevention program sustainability
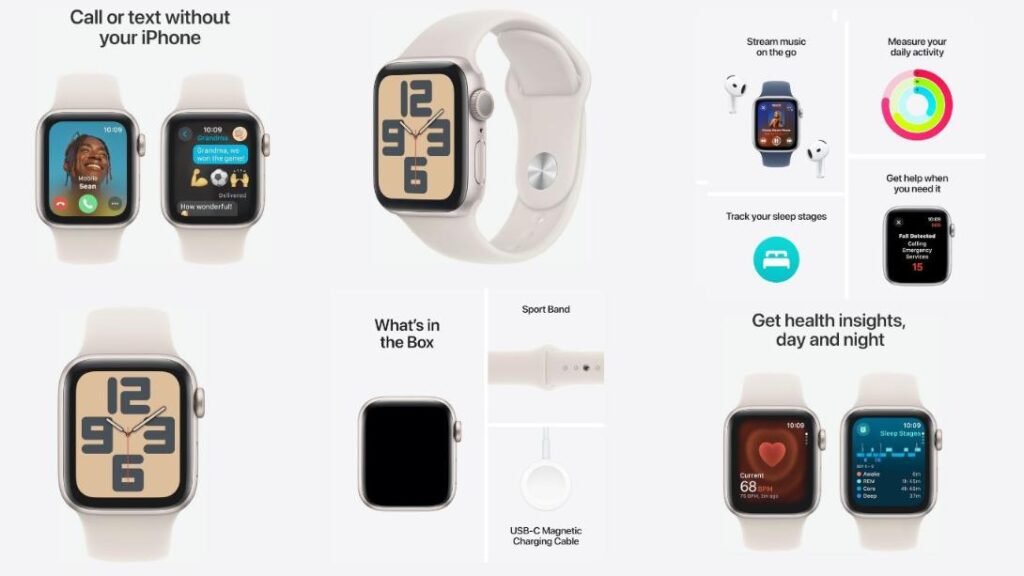
Technology and Healthcare Access
Digital solutions might help bridge some gaps. New technologies offer ways to reduce costs while maintaining care quality.
Promising developments include:
- Expanded telemedicine options
- Health monitoring apps
- Online prescription services
- Virtual support groups
- Digital health records access
Employer Healthcare Changes
Companies face decisions about employee health benefits. Many employers explore new ways to provide healthcare support.
Workplace adaptations include:
- Enhanced wellness programs
- Direct primary care arrangements
- Health savings account contributions
- On-site medical services
- Preventive care incentives
Community Support Networks
Local communities develop support systems. These networks help residents navigate healthcare changes.
Support mechanisms include:
- Healthcare navigation assistance
- Medical bill negotiation services
- Prescription buying groups
- Volunteer transportation programs
- Emergency care funds
Long-term Healthcare Planning
Americans need new approaches to long-term health planning. Financial experts suggest several strategies for future healthcare needs.
Planning elements include:
- Medical savings strategies
- Insurance combination approaches
- Healthcare proxy arrangements
- Advanced care directives
- Asset protection plans
International Comparisons
Other countries offer insights into healthcare system changes. Their experiences provide valuable lessons for Americans facing similar challenges.
Learning points include:
- Successful cost control measures
- Public-private partnership models
- Preventive care approaches
- Healthcare delivery innovations
- Patient support systems
Conclusion
While healthcare developments present problems, knowing and planning can help you handle them. Communities that collaborate can develop inventive solutions. The goal is to be educated and plan ahead of time, while also helping those who will be most affected by these changes.
Frequently Asked Questions
When will the budget changes take effect?
The implementation date is still being discussed, but modifications are expected to begin in the following fiscal year.
How should I prepare for possible coverage changes?
Begin studying choices, making savings, and discussing strategies with your healthcare doctors.
How will these changes impact emergency medical care?
Emergency services must still offer care, but the price and coverage may alter.
What options exist if I lose current coverage?
Look into community health centers, state programs, and healthcare marketplaces for alternatives.
How might state healthcare programs change?
States might adjust their programs differently, depending on local needs and resources.
Will children’s healthcare programs face cuts?
While children’s programs might see changes, many proposals aim to protect essential pediatric services.
Can healthcare providers assist with cost management?
Many doctors provide payment options and sliding scale pricing to patients who are struggling financially.
What resources can help me manage these changes?
Healthcare advocates, social workers, and community organizations can offer advice and assistance.
How can healthcare technology assist lower costs?
Digital health solutions can improve service efficiency and accessibility while potentially cutting overall costs.
What role do employers play in healthcare changes?
Many employers are adapting their benefits packages and exploring new ways to support employee health.
How can communities work together to support healthcare needs?
Local groups often create support networks, sharing resources and information to help residents access care.
What can we learn from other countries’ healthcare systems?
International examples show various approaches to balancing cost control with quality care.
How might mental health services change?
Mental health coverage could see significant adjustments, affecting both treatment access and cost.